🧭 Why Risk Management is Critical for MedTech Success
Risk management serves as a strategic tool that safeguards patients, enhances product quality, and mitigates regulatory risk.
A successful risk management process is essential whether you are submitting a device to the FDA or seeking EU MDR approval.
✅ Prevent product recalls and patient injury
✅ Improve the usability and safety of your design
✅ Strengthen your Technical Documentation and post-market surveillance.
✅ Make audits and inspections easier by Notified Bodies or FDA investigators
✅ Harmonize your product lifecycle to ISO 14971:2019
📌 Don’t miss our related guides:
- Post-Market Surveillance (PMS) for Medical Devices: Essential Roadmap to Compliance and Market Leadership
- CAPA Success Made Easy: Your Step-by-Step Guide to FDA and EU MDR Compliance for MedTech Companies
🚦 What Is Risk Management for Medical Devices?
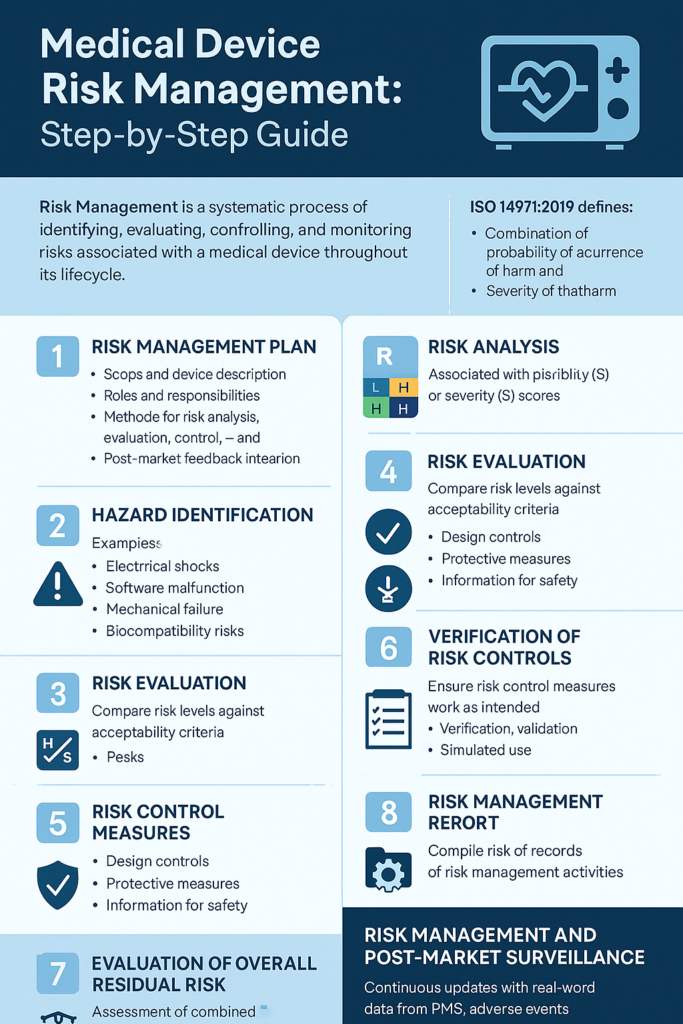
Risk management is a planned, evidence-based procedure that creates, analyzes, minimizes, and monitors potential medical device risks.
Risk, as defined by ISO 14971, is
“Combination of the probability of occurrence of harm and the severity of that harm.”
This process addresses risks related to design, production, clinical application, software, and cybersecurity. Risk management is also a process; it starts in development and goes on in the post-market existence of the device.
🚀 Step-by-Step Risk Management Process (ISO 14971 Aligned)
Here is your whole template for developing a compliant risk management system:
✅ 1. Risk Management Plan (RMP)
What It Is:
A Risk Management Plan (RMP) sets the strategy and scope for your risk process. The “project blueprint” defines how you will manage, monitor, and evaluate risks.
Include in Your RMP:
- Device description and intended use
- Risk acceptability criteria
- Risk analysis and evaluation methods
- Roles and responsibilities
- Documentation and review schedules
- Integration with PMS and CAPA systems
Why It Matters:
Without a detailed plan, your risk process will not be consistent, and regulators will find it inadequate.
✅ Internal Link: Find out how to reference your technical documentation to PMS and risk.
✅ 2. Hazard Identification
What It Is:
Identify all the potential causes of harm related to your medical device, for example:
- Biological (e.g., toxic materials)
- Electrical (e.g., shock, EMI)
- Mechanical (e.g., Failure of parts)
- Software (e.g., defects in firmware)
- Usability (e.g., incomprehensible interfaces)
- Environmental (e.g., overheating)
Tools You Can Use:
PHA (Preliminary Hazard Analysis)
FMEA (Failure Mode and Effects Analysis)
Task Analysis (for usability hazards)
Why It Matters:
If you do not detect a hazard, you cannot analyze or control it, risking your device’s failure or recall.
✅ Internal Link: Read more about design verification and validation strategies.
✅ 3. Risk Analysis
What It Is:
After you have found hazards, score each risk by
Severity (S): How severe is the damage?
Probability (P): How probable is it to happen?
Plot a risk matrix to label risks as low, medium, or high graphically.
Example:
| Hazard | Severity | Probability | Risk Level |
|---|---|---|---|
| Battery Overheating | Major | Occasional | High |
Why It Matters:
Numbering risk helps determine what dangers must be controlled and what can be monitored.
✅ 4. Risk Evaluation
What It Is:
Determine whether the evaluated risk is acceptable according to the criteria defined in the RMP.
If acceptable, proceed with control monitoring.
If unacceptable, implement mitigation measures.
Why It Matters:
You must show regulators that your device meets a justified and documented degree of safety.
✅ 5. Control Measures for Risk
What It Is:
Install measures to deal with unacceptable risks by:
Design alterations (e.g., safer material for containment)
Protective measures (e.g., warning devices)
Safety information (e.g., better instructions)
Important:
Having implemented a control, decide if it:
Introduced new risks
Lessened original risk as desired
It is acceptable as per residual risk assessment
Why It Matters:
Risk control is not just a case of adding warnings—it has to be quantifiable risk reduction.
✅ 6. Verification of Risk Controls
What It Is:
Demonstrate that your controls worked by design verification, bench testing, or software validation.
Examples:
Pass/fail safety limit testing
Usability test to validate instruction clarity
Software test to validate bug fix effectiveness
Why It Matters:
Regulators require proof, not a promise, that your risk controls work.
✅ 7. Overall Residual Risk Evaluation
What It Is:
After having included all controls, evaluate the overall residual risk and ask yourself:
Is the residual risk acceptable?
If not, can you defend it based on the benefit-risk ratio?
Are PMS or clinical data in favor of defending?
Why It Matters:
Your product should work and continue to be safe when used as intended, even after considering all anticipated hazards.
✅ Internal Link: Cross-reference this step to your Post-Market Surveillance Plan for lifecycle refreshes.
✅ 8. Risk Management Report (RMR)
What It Is:
This report provides a comprehensive overview of all your risk management activities.
- Devices covered
- Risk analysis summary
- Residual risk evaluation
- Verification results
- CAPA and PMS relationships
Why It Matters:
The RMR is auditor-proof evidence of an end-to-end and compliant risk system.
✅ 9. Risk Management File (RMF)
What It Is:
The master file includes
- Risk Management Plan
- Hazard and risk analyses
- Verification evidence
- Risk Control decisions
- Risk Management Report
- PMS + CAPA integration records
Why It Matters:
It is confirmed during FDA inspections and by Notified Bodies as part of your technical documentation.
🔄 Risk Management and Post-Market Surveillance (PMS)
Why it matters
Risk management does not stop once the product is released—it needs to stay current with actual use in the field.
Add:
- Complaint trends
- Adverse event reports
- Field corrective actions (FSCA)
- Clinical follow-up (PMCF) outcomes
CAPA findings
⚠️ Common Mistakes to Avoid
❌ Using risk management as a one-time report
❌ Copying and pasting risk matrices between products
❌ Ignoring usability risks and user error
❌ Failing to include post-market data in RMF
❌ Failure to check the efficacy of risk controls
🏆 Best Practices for Risk Management
✅ Involve RA/QA, engineering, clinical, and usability experts
✅ Leverage digitized RMF systems for traceability
✅ Schedule RMF reviews routinely into Management Review calendars
✅ Train your teams in risk-based thinking
