🧭 Definition: A Clear Starting Point for Absolute Beginners (FDA & EU MDR)
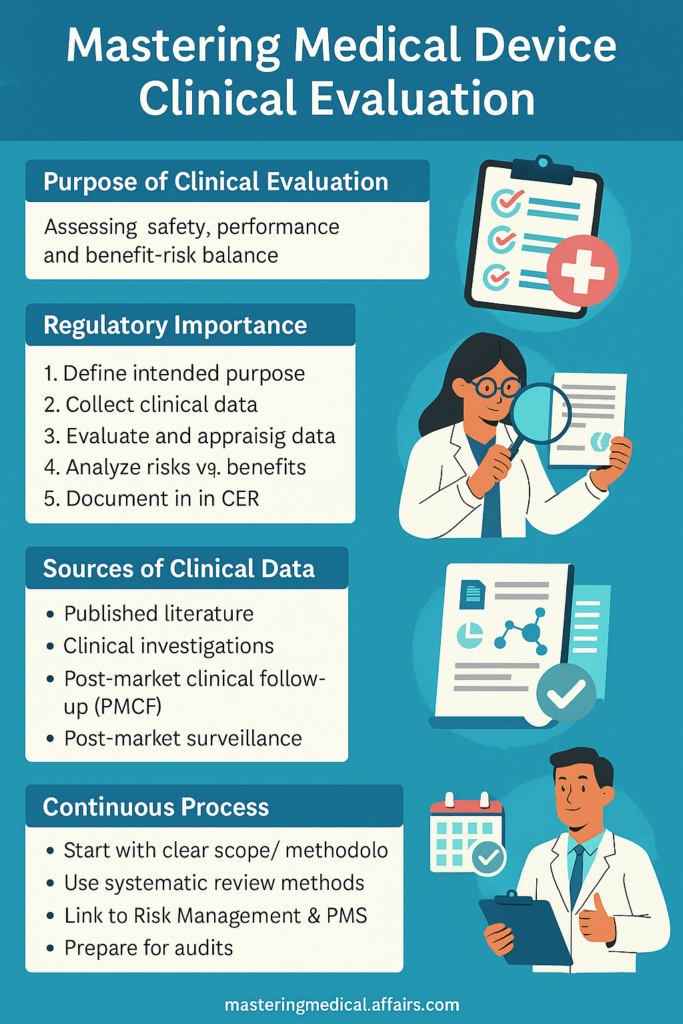
Clinical evaluation is the process of showing a medical device is safe and effective for patients before and after it’s sold.
- Suppose you have developed a new type of insulin pump. Before it gets used, you have to show regulators that
- It functions as intended (performance).
- It won’t cause unintended damage (safety).
- Medical benefits overstate any danger (benefit-risk analysis).
This type of testing is not optional—it’s a legal requirement in most countries, including the United States and the European Union.
Clinical evaluation ensures that
- Protect patients
- Doctors, physicians, and hospitals trust your product
- Regulators (e.g., the FDA) or Notified Bodies approve your device
It works for
- Marketing authorization (CE marking or FDA clearance)
- Avoiding recalls, liability suits, or regulatory penalties
📝 Why evaluation important for ensuring regulatory compliance??
✅ For EU MDR (European Union Medical Device Regulation):
As per EU MDR 2017/745, clinical evaluation is a must for all medical devices.
This is legislated by law in Annex XIV and therefore a strict mandate
If evaluation is not conducted properly:
- You cannot get CE Marking
- You cannot sell your device in the EU legally
✅ For FDA (United States):
The FDA doesn’t ask for a formal “Clinical Evaluation Report” like the EU does.
but they do require sound evidence, especially for
- High-risk devices (PMA submissions)
- New devices (De Novo requests)
- Devices needing human performance data in 510(k)
Not meeting clinical evidence standards may result in:
- Rejected applications
- Delayed market entry
- Potential enforcement actions
🚦 Could you please explain what it is actually involves?
Let’s break it down into elementary, beginner-stage steps:
✅ Step 1: Define Your Medical Device and Its Intended Use
Even before you start assessing anything, you have to have a clear answer to:
- What does your device do?
- Who is it for?
- What condition does it treat, monitor, or diagnose?
- How is it used (by doctors, patients)?
This is called the Intended Purpose, and it serves as the foundation of your overall clinical evaluation.
✅ Step 2: Collect Data
You have to collect real-world data from credible sources. These can be
📄 Published Scientific Literature:
- Research articles in medical journals
- Studies on your device or similar devices
- Reviews that show safety, performance, and clinical outcomes
🧪 Clinical Investigations
- Controlled trials you sponsor to assess your device
- Conducted in line with rigorous ethics requirements (e.g., ISO 14155)
- Usually needed for new, high-risk devices
📝 Post-Market Clinical Follow-Up (PMCF):
- Data collected after the device has been sold and used in real patients
- Includes performance reports, complaints, or adverse events
🗂️ Post-Market Surveillance (PMS) Data:
- Incident reports, user feedback, complaint trends, device malfunctioning
✅ Step 3—Evaluate and Appraise the Data You Collected
You can’t just collect data—you need to analyze it critically.
- Is the data relevant to your device?
- Is it high-quality, free from bias, and statistically representative?
- Does it suggest both safety and performance?
- Are there gaps in knowledge?
You should use systematic review methods—such as the PRISMA method—to ensure your evaluation is structured, transparent, and defensible.
✅ Step 4—Write a Clinical Evaluation Plan (CEP)
Before starting your evaluation, create a CEP that outlines
- The objectives of your evaluation
- What data sources you’ll use
- How you’ll judge the quality of each study or report
- How you’ll decide if benefits outweigh risks
Why this matters:
The regulators require proof that you didn’t cherry-pick information.
A CEP shows you had a systematic, unbiased methodology from the start.
✅ Step 5—Analyze Risks vs. Benefits
This is where you weigh the pros and cons:
- What is the device’s medical value?
- What are the identified or possible risks?
- Does the benefit outweigh the risk for patients?
You must give the clear, scientific case regulators can understand.
✅ Step 6—Document Everything in a Clinical Evaluation Report (CER)
EU MDR needs a CER with
- Your summary of clinical data
- Analysis of your data
- Benefit-risk conclusions
- How you will still be monitoring safety after the launch
The CER is an officially required document reviewed by your Notified Body.
🇪🇺 EU MDR Evaluation Requirements—Explained Clearly
A CER is necessary for all devices, including low-risk devices.
High-risk devices usually require new clinical studies.
You have to keep your CER up-to-date with new information (referred to as the “living document” strategy).
If you are claiming your device is similar to another one, you need to demonstrate this with
- Clinical similarity
- Technical similarity
- Biological safety similarity
- Having access to the data for the other device
This is much more stringent than under the previous EU MDD system.
🇺🇸 FDA Requirements—What You Need to Know
As opposed to the EU, the FDA is interested in
- Data included in PMA, De Novo, or 510(k) submissions
- Clinical trials under the IDE (Investigational Device Exemption)
Real-world evidence, if valid
- There’s no such document as an “FDA CER”, but you must include strong clinical evidence when:
- The device is a Class III high-risk device
- You’re submitting a new claim
- Preclinical testing is inadequate
🔄 Why Clinical Evaluation Is a Continuous Process—Not a One-Time Task
Many companies mistakenly believe
“We wrote a CER… done!”
Nope.
Your clinical evaluation must be
- Updated continuously with current clinical evidence
- Merged with Post-Market Surveillance and Risk Management
- Ready at all times for audit or regulatory inspection
- Should post-market data reveal new failures or risks, your CER will require adjustments.
⚠️ Common Mistakes Beginners Make
❌ Believing clinical studies are not required for low-risk devices
❌ Believing literature reviews are sufficient
❌ Failing to clearly define the methods of evaluation within the CEP
❌ Duplicate outdated data or other reports by your company
❌ Not updating the CER after launch
✅ Best Practices for a Successful Evaluation
✅ Start with a precise intended use and patient population
✅ Use systematic, clear review procedures (like PRISMA)
✅ Describe your methods clearly in the CEP and CER
✅ Include regulatory affairs experts early to advise
✅ Pair Clinical Evaluation with Risk Management, PMS, and PMCF
✅ Keep your CER available to audit at all times
📚 References
- EU MDR 2017/745 Annex XIV – Clinical Evaluation Requirements
- MEDDEV 2.7/1 Rev. 4 – EU Clinical Evaluation Guidelines
- FDA Guidance on Clinical Data for Medical Devices
- ISO 14155 – Good Clinical Practice for Medical Device Trials
You may also like to read
Medical Device Risk Management: The Step-by-Step Guide to FDA and EU MDR Compliance????
